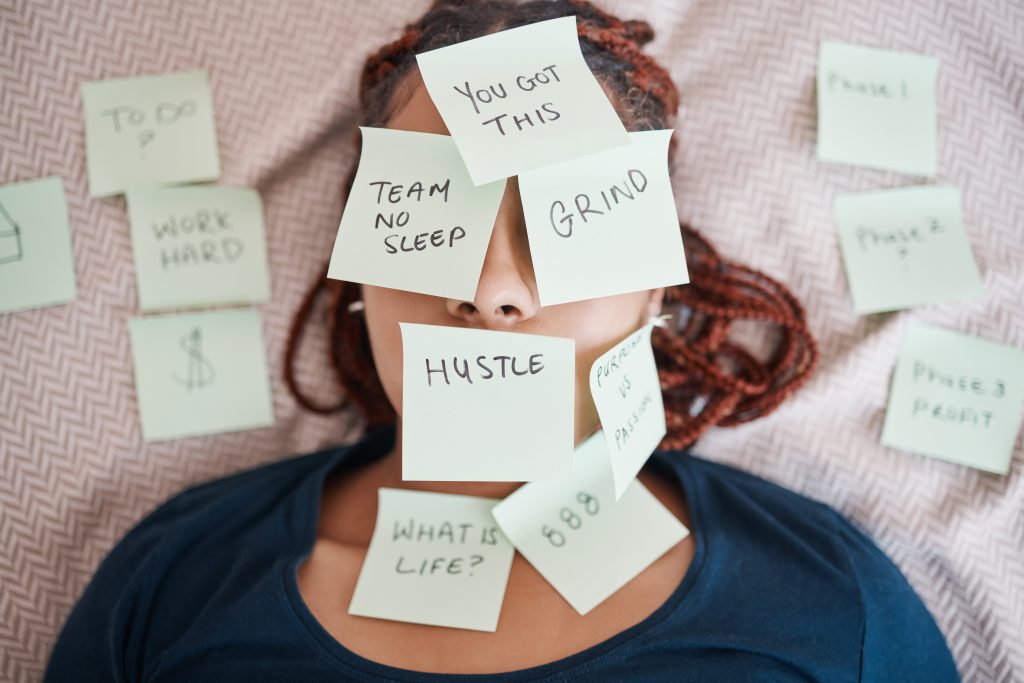
We’ve all been there. That nagging concern that’s been sitting in the back of your mind for weeks—maybe months. The sleep issues that started as “just a rough patch.” The persistent stress that you’ve convinced yourself is just part of modern life. The general tiredness you’ve attributed to being busy.
“I’ll book an appointment next week,” you tell yourself. “When things calm down a bit.”
But next week becomes next month, and suddenly you’re six months down the track, still carrying that same worry, still making the same promises to yourself about “getting it sorted.”
If this sounds familiar, you’re not alone. Millions of Australians are stuck in the cycle of healthcare procrastination—and it’s costing them far more than they realise.
The true price of avoiding medical consultations isn’t just about delayed treatment. It’s about the compound effect of living with uncertainty, the productivity lost to untreated concerns, and the way small issues can snowball into significant problems when left unaddressed.
Here’s the uncomfortable truth: the cost of procrastination often exceeds the cost of action—sometimes by a considerable margin.
The Psychology Behind Healthcare Procrastination
Let’s start with the elephant in the room: why do we avoid seeking medical help when we know we should?
The answer isn’t as simple as laziness or ignorance. Healthcare procrastination is a complex psychological phenomenon driven by several deeply human tendencies.
Fear and the Unknown
Most healthcare avoidance stems from fear—not just of bad news, but of the unknown. Our minds are incredibly creative when it comes to imagining worst-case scenarios. That persistent headache becomes a brain tumour. The irregular sleep pattern becomes a sign of serious mental health issues.
The irony? The uncertainty of not knowing often creates more anxiety than the reality of knowing. Yet our brains are wired to avoid potential threats, even when avoiding them creates greater stress.
The “It’s Probably Nothing” Trap
On the flip side, we’re masters of minimisation. We convince ourselves that symptoms aren’t serious enough to warrant professional attention. This optimism bias serves us well in many areas of life, but it can be counterproductive when it comes to health.
The result? We wait for symptoms to become “bad enough” to justify seeking help—often meaning we wait until problems are harder to address.
The Inconvenience Factor
Here’s where it gets really interesting: research shows that convenience plays a massive role in healthcare decisions. The more barriers between you and getting help, the more likely you are to postpone seeking it.
Traditional healthcare presents numerous friction points:
- Booking delays: Waiting weeks for available appointments
- Time disruption: Taking half a day off work for a 15-minute consultation
- Travel and waiting: The logistics of getting to and from appointments
- Scheduling complexity: Coordinating your calendar with limited appointment slots
Each barrier makes procrastination more attractive and action more daunting.
The Mental Load Problem
Think about what’s involved in booking a traditional medical appointment:
- Remembering to call during business hours
- Navigating phone systems and hold times
- Coordinating schedules weeks in advance
- Arranging time off work
- Organising transport and parking
- Managing the disruption to your entire day
That’s exhausting before you even step foot in a waiting room.
No wonder we postpone. The mental load of accessing healthcare can feel overwhelming when you’re already dealing with health concerns.
The Financial Reality of Delayed Care
Now let’s talk money—because healthcare procrastination has serious financial implications that extend far beyond medical costs.
The Compound Interest of Health Problems
Small issues rarely stay small. That sleep problem you’ve been ignoring? Left unaddressed, it can develop into chronic fatigue, affecting your work performance and potentially requiring more intensive intervention down the track.
The stress you’ve been “managing” on your own? Chronic stress is linked to a range of physical health issues, from cardiovascular problems to digestive concerns. Early intervention is almost always more cost-effective than crisis management.
Lost Productivity and Performance
Here’s what many people don’t calculate: the ongoing cost of functioning below your optimal level.
Consider these hidden financial impacts:
- Reduced work performance due to fatigue, stress, or untreated concerns
- Increased sick days from preventable complications
- Mental energy drain from carrying unresolved health worries
- Decision fatigue from constantly weighing whether symptoms warrant attention
- Relationship strain from irritability or withdrawn behaviour due to untreated issues
A recent study found that employees with untreated sleep disorders cost their employers an average of $2,280 per year in lost productivity. That’s just one example of how individual health impacts extend beyond personal wellbeing.
The Emergency Room Effect
When we finally can’t ignore symptoms anymore, we often end up seeking help in crisis mode. Emergency department visits and urgent care consultations typically cost significantly more than routine preventive consultations.
More importantly, problems addressed in crisis mode often require more intensive treatment than those caught early. The financial difference between a routine consultation and emergency intervention can be substantial.
Workplace and Career Impacts
Untreated health concerns don’t just affect your current job performance—they can impact long-term career prospects. Chronic fatigue, unmanaged stress, or persistent discomfort can limit your capacity for career advancement, networking, and professional development.
The opportunity cost of operating below your potential compounds over time, potentially affecting earning capacity for years.
The Physical and Mental Health Cascade
Here’s where things get really concerning: health issues rarely exist in isolation.
The Interconnected Web of Symptoms
Sleep problems affect stress levels. Stress impacts physical health. Physical discomfort disrupts sleep. It’s a cycle that can spiral quickly when left unaddressed.
What starts as a manageable concern can evolve into a complex web of interconnected issues. Breaking the cycle early is infinitely easier than untangling it later.
The Quality of Life Tax
Living with unresolved health concerns creates a constant background drain on your mental and emotional resources. You might not realise how much energy you’re spending:
- Monitoring symptoms and wondering if they’re getting worse
- Making daily adjustments to accommodate discomfort or limitations
- Carrying the mental burden of unaddressed concerns
- Explaining away symptoms to yourself and others
- Avoiding activities or situations that might exacerbate problems
This “quality of life tax” accumulates daily, robbing you of energy, enthusiasm, and peace of mind.
The Social and Relationship Cost
Untreated health issues don’t just affect you—they impact your relationships. Partners worry. Family members notice changes in your mood or energy. Friends might feel you’re less present or engaged.
The irony? Often the people closest to you are urging you to seek help while you continue to postpone it.
Building Negative Health Patterns
Perhaps most concerning is how procrastination can become a learned pattern. Each time you successfully “tough it out” or “wait and see,” you reinforce the behaviour of avoiding professional consultation.
This can lead to increasingly poor health decisions and a growing disconnect from professional healthcare support.
The Convenience Barrier: Why Accessibility Matters
Here’s what we’ve learned from working with thousands of patients: when you remove barriers to accessing healthcare, people make better health decisions.
The Psychology of “Convenient” vs “Important”
Traditional healthcare asks you to treat medical consultations as urgent emergencies worthy of major life disruption, or ignore them entirely. There’s no middle ground for “important but not crisis-level” concerns.
This binary thinking doesn’t match how most health issues actually develop. Most problems benefit from timely attention without requiring emergency-level response.
How Telehealth Changes the Equation
When healthcare becomes as accessible as a video call, something interesting happens to decision-making patterns:
- Reduced friction means less reason to postpone
- Flexible scheduling accommodates life rather than disrupting it
- Immediate availability prevents issues from building up over time
- Comfort settings reduce anxiety around seeking help
- Follow-up ease encourages ongoing rather than crisis-driven care
The result? People address concerns earlier, when they’re easier to manage and less disruptive to daily life.
Breaking the “Perfect Timing” Myth
One of the biggest barriers to seeking healthcare is waiting for the “right time.” But there’s never a perfect time to address health concerns—there are only earlier and later opportunities.
Accessible healthcare helps you act on “good enough” timing rather than waiting for perfect conditions that may never arrive.
What Actually Happens When You Stop Avoiding
Let’s address the elephant in the room: what if you actually book that consultation you’ve been postponing?
The Relief Factor
The most common feedback we receive from patients isn’t about medical outcomes—it’s about relief. Simply talking through concerns with a qualified professional often provides immediate psychological benefits:
- Validation that your concerns are worth addressing
- Clarity about what you’re actually dealing with
- Direction on appropriate next steps
- Peace of mind from professional assessment
- Reduced anxiety from ending the uncertainty
Demystifying Professional Consultation
Here’s what actually happens during most consultations:
- Discussion of your concerns in a non-judgmental environment
- Review of your health history and current circumstances
- Professional assessment of your symptoms or concerns
- Clear explanation of potential causes or contributing factors
- Practical guidance on management approaches or next steps
- Follow-up planning to monitor progress or concerns
It’s typically far less intimidating and much more helpful than anticipated.
Common Outcomes of Addressing Concerns Early
The majority of health concerns that people procrastinate about fall into manageable categories:
- Lifestyle factors that can be addressed through education and gradual changes
- Treatable conditions that respond well to early intervention
- Normal variations that require reassurance rather than treatment
- Stress-related symptoms that benefit from professional guidance and support strategies
- Minor issues that can be prevented from becoming major problems
Early consultation often leads to simpler, less invasive solutions than waiting until problems escalate.
Building Better Health Habits
Perhaps most importantly, addressing concerns promptly helps establish a pattern of proactive rather than reactive healthcare. This shift can have long-term benefits that extend far beyond any individual consultation.
Practical Steps to Break the Avoidance Cycle
Ready to stop postponing and start addressing? Here are practical strategies to overcome healthcare procrastination:
Recognise Your Procrastination Patterns
Start by acknowledging your typical avoidance behaviours:
- Do you tell yourself you’re “too busy” for health concerns?
- Do you wait for symptoms to become “bad enough” to justify attention?
- Do you research symptoms online instead of seeking professional consultation?
- Do you make appointments but find reasons to cancel or postpone them?
Awareness is the first step to changing patterns.
Use Technology to Reduce Barriers
Modern healthcare doesn’t have to involve the traditional barriers that encourage procrastination:
- Online booking eliminates phone tag and business-hour restrictions
- Telehealth consultations remove travel and waiting room time
- Flexible scheduling accommodates your life rather than disrupting it
- Digital health records streamline information sharing and follow-up care
The easier it is to access care, the less likely you are to postpone it.
Embrace “Good Enough” Timing
Stop waiting for the perfect time and start acting on “good enough” timing:
- Book consultations during routine planning rather than when symptoms peak
- Use lunch breaks or quiet periods for telehealth appointments
- Schedule follow-up consultations while current concerns are top of mind
- Remember: addressing concerns early is almost always easier than addressing them late
Make Health Consultations Routine
Shift from crisis-driven to routine healthcare patterns:
- Regular check-ins prevent issues from building up
- Seasonal health reviews catch problems before they escalate
- Stress and lifestyle consultations during busy periods
- Follow-up appointments to monitor ongoing concerns
Routine healthcare is far less stressful than emergency healthcare.
Start Small and Build Confidence
If healthcare anxiety is holding you back, start with lower-stakes consultations:
- Use preliminary screenings to get comfortable with the process
- Begin with general health discussions rather than specific symptom focus
- Build positive experiences with healthcare providers to reduce future avoidance
- Remember: most consultations are straightforward and helpful
The Real Cost of Waiting
Let’s bring this full circle. Healthcare procrastination isn’t just about delayed medical treatment—it’s about the compound cost of living with uncertainty, operating below your potential, and allowing manageable concerns to become complex problems.
The Investment Perspective
Think of healthcare consultations as investments rather than expenses:
- Early consultation typically costs less than delayed intervention
- Professional guidance can prevent minor issues from becoming major problems
- Peace of mind has value that extends beyond immediate health outcomes
- Improved quality of life affects every aspect of your daily experience
The return on investment for proactive healthcare is typically substantial.
Breaking the Cycle
Every time you postpone addressing a health concern, you’re making a decision—and that decision has consequences. You’re choosing uncertainty over clarity, worry over peace of mind, and potential complications over early intervention.
But here’s the empowering truth: you can break this cycle at any time.
Modern healthcare, particularly accessible telehealth services, removes most of the traditional barriers that encourage procrastination. When healthcare becomes convenient, timely, and accessible, postponing becomes the harder choice.
Your Next Step
If you’ve been putting off addressing a health concern—whether it’s sleep issues, stress, general health questions, or persistent symptoms—consider this your gentle reminder that waiting rarely improves outcomes.
The consultation you’ve been postponing might be simpler, more helpful, and more reassuring than you anticipate. The cost of continued procrastination often exceeds the cost of taking action.
Your health concerns are valid. Your peace of mind matters. And the “perfect time” to address them is almost always now rather than later.
This article provides general health information and should not replace professional medical advice. If you have specific health concerns, please consult with a qualified healthcare practitioner. All consultations should be conducted with AHPRA-registered medical professionals.