Let’s talk about the conversation that doesn’t happen.
You know the one. The whispered concern about a colleague who’s always “celebrating” something. The family dinner where everyone pretends not to notice that someone’s had a few too many again. The prescription bottle that’s somehow empty faster than it should be. The friend whose weekend stories increasingly revolve around substances that used to be just for special occasions.
Or maybe it’s simpler than that. Maybe it’s the conversation you’re not having with yourself.
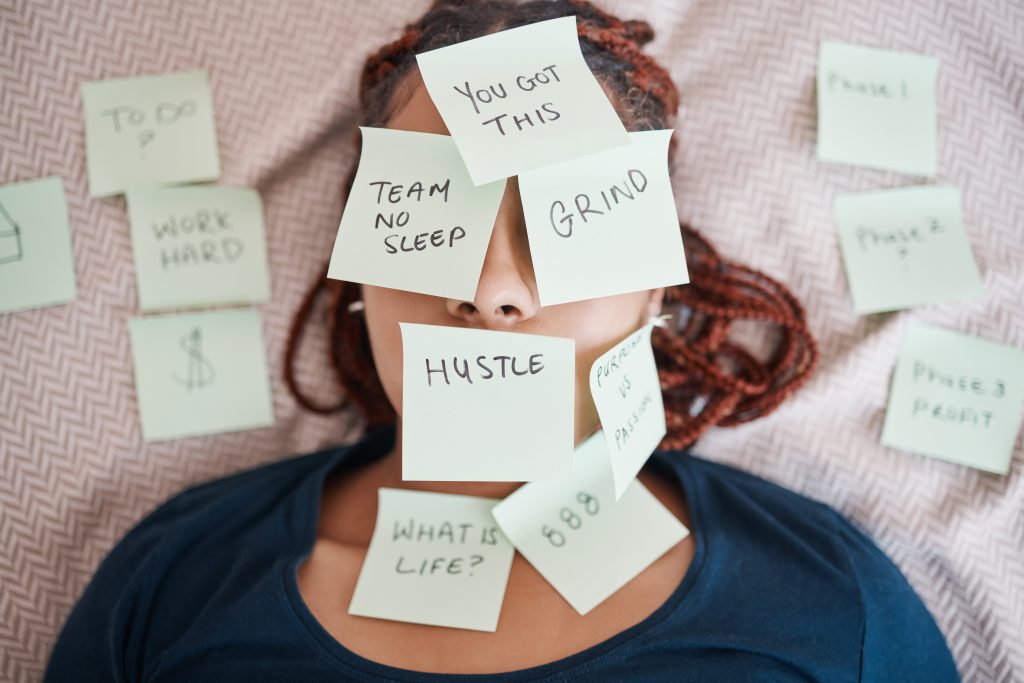
“I can handle this.”
“Everyone drinks like this.”
“It’s not that bad.”
“I’m still functioning fine.”
Here’s what’s interesting about these internal monologues: they’re usually happening precisely when someone would benefit most from an external perspective.
We’ve created this bizarre cultural framework where seeking help for addiction concerns is treated as admitting catastrophic failure, while simultaneously normalising behaviours that, in any other context, we’d recognise as problematic. It’s like deciding that you can only go to the doctor for broken bones if they’re sticking out of your skin.
But here’s the uncomfortable truth that the addiction industry doesn’t want to advertise, and that our “tough it out” culture certainly doesn’t want to acknowledge: most people who benefit from professional support for addiction concerns don’t look anything like what you think addiction looks like.
They’re high-functioning professionals. Devoted parents. University students. Retirees managing chronic pain. People whose lives would appear enviable from the outside, but who are quietly struggling with patterns they can’t seem to change on their own.
The real conversation about addiction isn’t about rock bottom—it’s about recognising when you could use some help climbing back up.
The Myths That Keep Smart People Making Dumb Decisions
Let’s start by destroying some of the mythology that prevents perfectly intelligent people from seeking help when they actually need it.
Myth #1: You Need to Lose Everything First
This is perhaps the most dangerous piece of fiction we tell ourselves about addiction: that professional help is only warranted after you’ve lost your job, your family, your health, or your home.
It’s the equivalent of saying you can only treat high blood pressure after you’ve had a heart attack. It’s not just wrong—it’s actively harmful.
The “rock bottom” narrative is compelling because it makes a great story, but it’s terrible healthcare strategy. Early intervention in addiction is like early intervention in any other health condition: more effective, less disruptive, and significantly less costly than crisis management.
Yet we’ve somehow convinced ourselves that seeking help before things become catastrophic is… what? Premature? Dramatic? Self-indulgent?
Here’s a radical idea: if something is affecting your quality of life, your relationships, your work, or your peace of mind, that’s enough reason to seek professional input. You don’t need to wait for permission from circumstance.
Myth #2: It’s About Willpower
This one’s particularly insidious because it sounds so reasonable. “Just stop.” “Have some self-control.” “Make better choices.”
If addiction were a willpower problem, intelligent, successful, disciplined people wouldn’t struggle with it. But they do. Constantly.
Addiction involves changes to brain chemistry, reward pathways, and decision-making processes. Trying to overcome addiction through willpower alone is like trying to overcome diabetes through positive thinking. It misunderstands the fundamental nature of what you’re dealing with.
The people who successfully address addiction concerns don’t have superior willpower—they have better strategies, professional support, and evidence-based approaches. They work smarter, not just harder.
Myth #3: You’ll Know When You Need Help
This might be the most dangerous myth of all: the idea that addiction announces itself clearly and that you’ll have obvious, unmistakable recognition when professional help becomes necessary.
The reality? Addiction is exceptionally good at convincing you that you don’t have addiction.
It’s the condition that tells you that you don’t have the condition. It’s the problem that insists it’s not a problem. It’s remarkably skilled at providing justifications, rationalisations, and explanations that sound perfectly reasonable—especially to the person doing the explaining.
“I only drink wine.”
“It’s prescribed by my doctor.”
“I function perfectly well.”
“Everyone at work does this.”
“I never drink before 5 PM.”
These statements might all be technically true while completely missing the point.
Myth #4: Professional Help Means Dramatic Life Overhaul
The all-or-nothing thinking around addiction treatment prevents many people from seeking help because they can’t envision fitting residential rehab into their existing responsibilities.
But here’s what most people don’t realise: the majority of addiction support doesn’t involve dramatic life disruption, residential treatment, or public disclosure.
Modern addiction support includes:
- Educational consultations that help you understand patterns and options
- Outpatient counselling that fits around your existing schedule
- Medical management that addresses physical aspects of addiction
- Lifestyle modification support integrated into your daily routine
- Family consultation to address broader relationship impacts
Most professional addiction support is designed to enhance your existing life, not replace it.
The Recognition Problem
These myths don’t just prevent people from seeking help—they prevent people from recognising they might need it.
When addiction is portrayed as:
- Only affecting people who’ve lost everything
- Being overcome through willpower alone
- Announcing itself obviously
- Requiring dramatic treatment interventions
Smart people think: “That’s not me, so this isn’t addiction.”
But what if we reframed it? What if addiction is simply patterns of behaviour around substances or activities that have become difficult to control and are causing unwanted consequences?
Suddenly, the conversation becomes a lot more relevant to a lot more people.
The Hidden Scale of a “Rare” Problem
Let’s establish some context here, because one of the reasons people don’t seek help for addiction concerns is the misconception that these issues are rare or unusual.
The Numbers Game
Addiction concerns affect millions of Australians—but these numbers are consistently underreported because of shame, stigma, and the very myths we’ve just discussed.
What we do know:
- Alcohol-related concerns affect a substantial portion of Australian adults
- Prescription medication dependency has increased dramatically
- Behavioural addictions are increasingly recognised and prevalent
- Most people experiencing addiction concerns appear high-functioning to outside observers
These aren’t statistics about “other people”—they represent colleagues, family members, friends, and possibly the person reading this article.
The Functional Addiction Reality
Perhaps the most overlooked category involves people who maintain their external responsibilities while privately struggling with substance use or behavioural patterns.
High-functioning addiction looks like:
- Successful career performance while using substances to cope with stress
- Maintaining family responsibilities while privately battling dependency concerns
- Meeting social expectations while experiencing internal distress about patterns
- Academic achievement that masks developing problems with substances
The functionality isn’t evidence that there’s no problem—it’s often evidence of how much energy is being expended to maintain the appearance of normalcy.
The Normalisation Problem
One reason addiction concerns often go unaddressed is that problematic patterns become normalised within certain contexts:
Professional Cultures:
- Industries where heavy drinking is expected or celebrated
- Prescription medication use that gradually escalates beyond medical necessity
- Work stress that’s “managed” through substance use
Social Contexts:
- Friend groups where substance use is the primary social activity
- Family systems where problematic patterns are generational
- Cultural celebrations that emphasise consumption
This normalisation creates a warped perspective where clearly problematic behaviour appears normal because it’s common within your reference group.
But here’s the thing: common doesn’t mean healthy, and widespread doesn’t mean acceptable.
The Real Cost of “Managing” on Your Own
Let’s talk about what “managing” addiction concerns actually costs—because the price tag goes far beyond the obvious.
The Daily Tax You Don’t Calculate
When you’re “managing” addiction concerns independently, you’re paying a daily tax that you probably don’t fully recognise:
Mental Energy Drain:
- Constantly monitoring and controlling your behaviour
- Managing anxiety about patterns you can’t quite control
- Explaining away concerns to yourself and others
- Carrying the weight of secrets and private struggles
Performance Impact:
- Reduced cognitive function from substance use or withdrawal
- Decreased emotional regulation affecting relationships and work
- Physical symptoms that require ongoing management
- Sleep disruption that compounds everything else
Decision Fatigue:
- Daily negotiations with yourself about use patterns
- Constant recalculation of what’s “acceptable” or “normal”
- Energy spent on justification and rationalisation
- Mental resources diverted from other priorities
This isn’t a minor inconvenience—it’s a substantial ongoing drain on your most valuable resources.
The Compound Interest of Problems
Addiction concerns rarely stay contained to one area of life—they tend to create cascading effects that compound over time:
Relationship Deterioration:
- Trust erosion with family and friends
- Increased conflict and misunderstanding
- Social isolation and withdrawal
- Communication breakdown
Professional Consequences:
- Decreased performance and reliability
- Missed opportunities and limited advancement
- Workplace conflicts and relationship strain
- Career reputation impacts
Health Complications:
- Physical health impacts from substance use
- Mental health deterioration from ongoing stress
- Sleep and nutrition disruption
- Increased risk of accidents and injuries
The longer these issues remain unaddressed, the more complicated and expensive they become to resolve.
The Prevention Economics
Here’s what the rehabilitation industry doesn’t want you to think about: early intervention is almost always more effective and less disruptive than crisis management.
Early Professional Support Might Include:
- Educational consultation about patterns and health impacts
- Strategies for monitoring and modifying behaviour
- Medical assessment and ongoing monitoring
- Counselling support for underlying concerns
Crisis Intervention Often Requires:
- Emergency medical intervention
- Intensive residential treatment
- Employment and relationship crisis management
- Legal and financial consequence management
The difference in cost, disruption, and effectiveness is substantial.
What Professional Help Actually Looks Like (Spoiler: It’s Not What You Think)
Most people avoid seeking help for addiction concerns because they have no idea what professional support actually involves—and their assumptions are usually wrong.
The Reality of Professional Consultation
Here’s what actually happens when you seek professional help for addiction concerns:
Initial Consultation:
- Confidential discussion of your specific concerns and circumstances
- Assessment of patterns, impacts, and health considerations
- Information about options and approaches available
- Collaborative discussion of goals and preferences
- No judgment, no lectures, no dramatic interventions
It’s more like consulting with a specialist about any other health concern than like the intervention scenes you’ve seen in movies.
The Collaboration Model
Effective addiction support is collaborative rather than prescriptive:
- You maintain control over decisions about your treatment and goals
- Your preferences matter in determining approaches and interventions
- Your expertise about your own life is recognised and valued
- Progress is measured against your goals, not generic benchmarks
- Flexibility is built in to accommodate changing needs and circumstances
This isn’t about surrendering control—it’s about gaining support and expertise to enhance your existing efforts.
The Medical Approach
Professional addiction support treats addiction as a health condition requiring medical intervention, not a moral issue requiring judgment:
- Evidence-based approaches proven to be effective
- Medical assessment of physical and mental health impacts
- Coordinated care that addresses addiction alongside other health concerns
- Privacy protections that maintain confidentiality
- Professional standards that ensure appropriate, non-judgmental care
This medical model removes shame and stigma from the equation.
The Options Menu
Professional addiction support isn’t one-size-fits-all—it’s tailored to individual circumstances:
Educational Support:
- Information about addiction, health impacts, and management strategies
- Guidance on self-monitoring and harm reduction approaches
- Resources for ongoing learning and self-management
Counselling Support:
- Individual therapy to address underlying concerns and develop coping strategies
- Family counselling to address relationship impacts
- Group support with others facing similar challenges
Medical Management:
- Medication-assisted treatment where appropriate
- Management of withdrawal symptoms
- Treatment of co-occurring physical and mental health conditions
Intensive Support:
- Day programs that allow continued work and family responsibilities
- Residential treatment for situations requiring intensive intervention
- Crisis intervention for immediate safety concerns
The level and type of support is matched to your specific needs and preferences.
The Accessibility Revolution: How Modern Healthcare Changes Everything
Traditional healthcare barriers have long prevented people from seeking help for addiction concerns—but modern healthcare delivery is changing this equation dramatically.
The Privacy Revolution
Telehealth consultation provides unprecedented privacy for addressing addiction concerns:
Environmental Control:
- Consultations from your own comfortable, private space
- No risk of being seen entering treatment facilities
- No waiting room encounters with people you might know
- Complete control over your physical environment during consultations
Reduced Exposure:
- Minimal people involved in the consultation process
- Digital rather than physical records in public spaces
- No front desk interactions or administrative exposure
- Reduced chance of accidental disclosure
This level of privacy can make the difference between seeking help and continuing to struggle alone.
The Convenience Factor
Accessible healthcare eliminates the practical barriers that often prevent addiction support:
Scheduling Flexibility:
- Appointments that fit around your existing responsibilities
- Early morning, evening, or weekend availability
- No travel time or transportation concerns
- Reduced disruption to work and family commitments
Geographical Freedom:
- Access to specialists regardless of your location
- Quality care in rural and remote areas
- No limitation to local provider availability
- Consistent care even with travel or relocation
This accessibility means practical concerns no longer need to prevent professional consultation.
The Comfort Advantage
The telehealth environment can reduce many psychological barriers to seeking help:
- Familiar surroundings that feel safer and more comfortable
- Physical distance that can reduce feelings of vulnerability
- Home advantage where you feel more in control
- Reduced intimidation from clinical settings and formal environments
These factors can make honest conversation about addiction concerns feel more manageable and less threatening.
The Follow-Up Revolution
Perhaps most importantly, telehealth makes ongoing support practical and sustainable:
- Regular check-ins without major life disruption
- Crisis support accessible when and where needed
- Consistent care that adapts to changing circumstances
- Long-term relationship building with healthcare providers
This ongoing accessibility supports sustained behaviour change rather than crisis intervention.
When to Stop Pretending You’ve Got This Under Control
The question isn’t whether you have an addiction problem—it’s whether you could benefit from professional support to address concerns you’re already aware of.
Quality of Life Indicators
Professional consultation can be valuable when addiction concerns are affecting your daily experience, even if they haven’t created obvious crises:
Daily Life Impacts:
- Difficulty fulfilling responsibilities you used to manage easily
- Reduced enjoyment of activities that were previously fulfilling
- Persistent worry about your patterns of use or behaviour
- Physical symptoms that interfere with comfort or performance
- Changes in sleep, mood, or energy related to substance use
These quality of life impacts are legitimate reasons for seeking professional input—you don’t need to wait for catastrophic consequences.
The Honesty Test
Here are some honest questions to consider:
- Do you think about your substance use or behaviour more than you’d like to?
- Have you made rules for yourself that you struggle to follow consistently?
- Do you feel like you need substances or behaviours to cope with stress, anxiety, or difficult emotions?
- Have people close to you expressed concerns about your patterns?
- Do you find yourself being defensive when the topic comes up?
- Are there activities or situations you avoid because of your use patterns?
If you answered yes to several of these questions, professional consultation could provide valuable insight and support.
The Prevention Opportunity
The most empowering realisation about addiction support is that you don’t need to wait for rock bottom—you can take action whenever you recognise that change would improve your life:
- Curiosity about your patterns is a legitimate reason for consultation
- Wanting to prevent problems is smarter than waiting for them to develop
- Quality of life concerns deserve professional attention
- Peace of mind has value beyond crisis prevention
Professional support is available not just when you’re in crisis, but whenever you could benefit from expert guidance.
Taking Action Without Drama
Ready to explore professional support without the drama, judgment, or life upheaval you might be imagining? Here’s how.
Start Where You Are
You don’t need to be “ready to change everything” to benefit from professional consultation:
- Information gathering is a legitimate goal for initial consultations
- Understanding your patterns can be valuable even if you’re not ready for major changes
- Exploring options doesn’t commit you to specific treatments
- Building relationships with healthcare providers can be helpful for future decisions
The goal is gaining insight and options, not immediate transformation.
The Low-Stakes Beginning
Initial addiction consultation is typically much less intense than people imagine:
- Confidential conversation about your concerns and circumstances
- Educational information about addiction, health impacts, and available support
- Assessment of current situation without pressure for immediate decisions
- Discussion of options based on your specific needs and preferences
Think of it as consulting with a specialist about health concerns rather than committing to dramatic life changes.
Managing the Control Concern
Many people worry that seeking professional help means surrendering control over their decisions and circumstances:
The reality is the opposite: professional support typically increases your control by:
- Providing information to make better-informed decisions
- Offering strategies to improve your ability to manage patterns
- Giving you additional options and resources
- Supporting your goals rather than imposing external goals
Professional support enhances your autonomy rather than replacing it.
Building Support Without Broadcasting
You can build professional support while maintaining privacy about your concerns:
- Medical confidentiality protects your privacy legally and professionally
- Selective disclosure allows you to share information only with people you choose
- Gradual approach lets you build comfort and trust over time
- Family support can be included at your discretion and timing
Seeking professional help doesn’t automatically mean everyone in your life will know about your concerns.
The Relief You Didn’t Know You Needed
Here’s what we’ve learned from thousands of consultations: the biggest surprise for most people isn’t what professional addiction support involves—it’s how much relief they feel just by taking action.
The End of Secrecy
Carrying addiction concerns alone is exhausting. The mental energy required to monitor, manage, justify, and hide patterns of behaviour creates a constant background drain.
Professional consultation provides:
- Validation that your concerns are legitimate and worth addressing
- Understanding of what you’re experiencing from someone with expertise
- Relief from carrying worries and questions alone
- Clarity about what you’re dealing with and available options
- Hope that change is possible with appropriate support
This psychological relief often provides immediate benefits even before implementing specific strategies.
The Perspective Shift
Professional support helps you see your situation from a different angle:
- Normalisation of struggles that felt isolating and shameful
- Context for understanding how addiction develops and persists
- Optimism based on evidence of successful outcomes for others
- Practical strategies that feel manageable rather than overwhelming
- Support that makes change feel possible rather than impossible
This perspective shift can be transformational even before behaviour changes occur.
The Empowerment Factor
Perhaps most importantly, professional support is empowering rather than disempowering:
- Knowledge about addiction science and effective approaches
- Skills for managing triggers, cravings, and difficult situations
- Strategies tailored to your specific circumstances and preferences
- Confidence that you can address concerns effectively
- Agency in making informed decisions about your health and wellbeing
Professional support doesn’t take control away—it gives you better tools for exercising control effectively.
The Uncomfortable Truth About Waiting
Here’s the final uncomfortable truth: there’s no good time to address addiction concerns, and there’s never a perfect moment to seek professional help.
There will always be work deadlines, family commitments, social obligations, and practical concerns that make “now” feel like poor timing.
But here’s what we know about timing and addiction: the best time to address concerns is when you first recognise them, not when they become impossible to ignore.
Early intervention is more effective, less disruptive, and more successful than crisis management. The consultation you’re postponing until “things calm down” might be exactly what helps things actually calm down.
Your Concerns Are Valid
If addiction concerns are affecting your quality of life, causing worry, or creating impacts you’d rather not have, they deserve professional attention—regardless of whether they match stereotypes or meet some arbitrary threshold of “serious enough.”
Your wellbeing matters. Your peace of mind has value. And the patterns you’ve been managing alone might be more manageable with professional support.
The Access Advantage
Professional addiction support has never been more accessible, private, or convenient than it is today. The barriers that might have prevented previous generations from seeking help have largely been removed by modern healthcare delivery.
There’s no longer a good reason to suffer alone when professional support is available, confidential, and designed to work around your life rather than disrupting it.
The conversation you’ve been avoiding with yourself might be the most important one you have this year.
This article provides general health information and should not replace professional medical advice. If you have specific concerns about addiction or substance use, please consult with a qualified healthcare practitioner. All consultations should be conducted with appropriately qualified medical professionals. In crisis situations, contact emergency services or crisis helplines for immediate support.