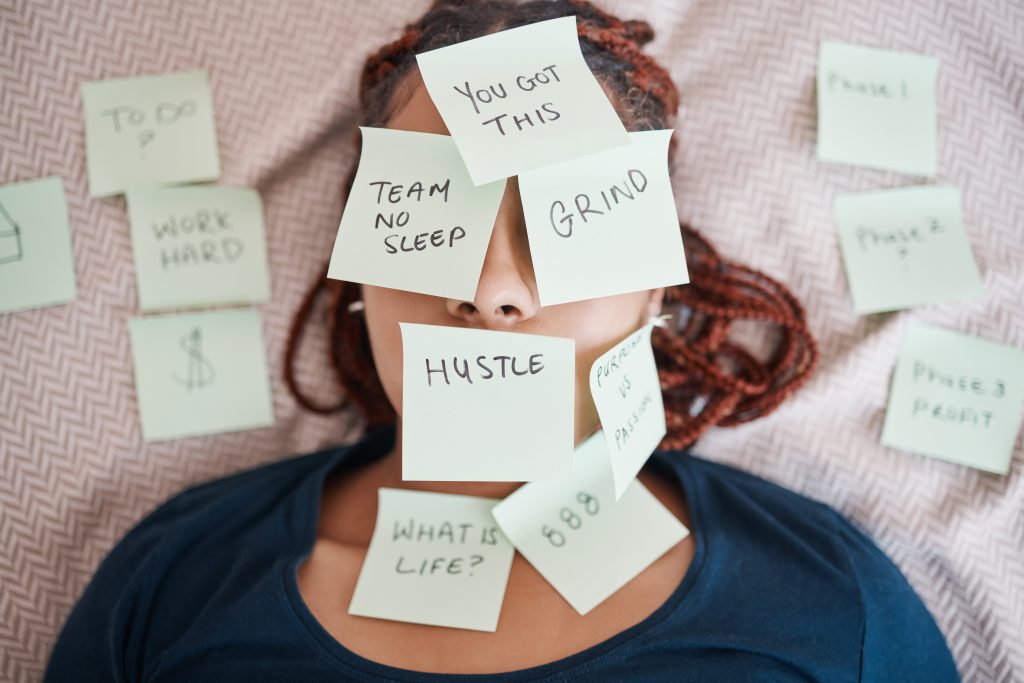
“It’s just stress.”
“It’s just a bit of trouble sleeping.”
“It’s just feeling a bit run down.”
How many times have you used the word “just” to dismiss a health concern? How often have you downplayed symptoms that are actually affecting your daily life, your relationships, your work performance—but somehow don’t seem “serious enough” to warrant professional attention?
We’ve created a peculiar hierarchy in how we think about health. Heart attacks and broken bones clearly deserve medical attention. But sleep problems? Stress? General fatigue or low mood? These get relegated to the “minor issues” category—problems we should handle on our own, push through, or simply accept as part of modern life.
Here’s what we’ve learned from thousands of consultations: the issues people dismiss as “minor” are often the ones creating the biggest impact on their quality of life.
Those sleep problems you’ve been managing for months? They’re not just about feeling tired. Chronic poor sleep affects everything from your immune system to your emotional regulation, from your cognitive performance to your physical health.
That stress you’ve normalised as part of your job or life circumstances? It’s not just psychological discomfort—it’s a physiological process that impacts virtually every system in your body.
The general health concerns you’ve been monitoring but not addressing? They rarely stay general, and they rarely resolve themselves.
The uncomfortable truth is this: we’ve been conditioned to ignore precisely the health issues that, when addressed early, can prevent bigger problems down the track.
The Interconnected Web: How Sleep, Stress, and Health Connect
Let’s start with a reality check: your body doesn’t operate in separate, isolated systems. Sleep, stress, and physical health aren’t independent concerns that can be addressed in isolation—they’re part of an intricate, interconnected web where each element influences all the others.
The Sleep-Stress Connection
Poor sleep doesn’t just make you tired—it fundamentally alters your stress response system. When you’re sleep-deprived, your body produces higher levels of cortisol, the primary stress hormone. This creates a vicious cycle: stress makes it harder to sleep, and poor sleep makes you more reactive to stress.
But it goes deeper than that. Sleep deprivation affects the prefrontal cortex—the part of your brain responsible for emotional regulation, decision-making, and impulse control. This means that when you’re not sleeping well, you’re literally less equipped to handle the daily stresses that would normally be manageable.
The Stress-Health Pipeline
Chronic stress isn’t just an emotional experience—it’s a physiological state that affects your entire body. When your stress response system is constantly activated:
- Your immune function decreases, making you more susceptible to illness
- Your digestive system becomes compromised, leading to gut health issues
- Your cardiovascular system works harder, increasing blood pressure and heart rate
- Your hormonal balance shifts, affecting everything from sleep to mood to metabolism
- Your muscle tension increases, leading to headaches, back pain, and general discomfort
These aren’t separate health problems—they’re manifestations of your body’s stress response.
The General Health Feedback Loop
Those vague feelings of being “not quite right”—low energy, frequent minor illnesses, difficulty concentrating, mood changes—often aren’t separate issues but symptoms of the same underlying imbalances.
When your sleep is poor and your stress levels are high, your body’s ability to maintain optimal function across all systems becomes compromised. The result? A cascade of seemingly unrelated symptoms that actually share common roots.
Why Treating Symptoms in Isolation Misses the Point
Here’s where traditional thinking about health gets it wrong: treating individual symptoms without addressing the interconnected system rarely provides lasting relief.
You might take something for the headaches, try a different pillow for the sleep problems, and attempt stress management techniques for the anxiety. But if you’re not addressing the underlying pattern of poor sleep, chronic stress, and compromised health, you’re essentially playing whack-a-mole with symptoms.
Professional consultation helps identify these patterns and address root causes rather than just managing symptoms.
Why We Dismiss What Matters Most
So if these issues are so interconnected and impactful, why do we consistently dismiss them as “minor”? The answer lies in a combination of cultural conditioning, normalisation, and misunderstanding about what constitutes legitimate health concerns.
The “Push Through” Culture
Australian culture, like many Western cultures, celebrates resilience and self-reliance. We’re conditioned to push through discomfort, to “tough it out,” and to view seeking help as a sign of weakness rather than wisdom.
This cultural programming serves us well in many situations, but it becomes counterproductive when it prevents us from addressing health issues that could be easily managed with early intervention.
The Normalisation Trap
When problems are common, we tend to assume they’re normal. Because sleep problems and stress are widespread, we’ve collectively decided they’re just part of modern life rather than health issues that deserve attention.
But common doesn’t mean normal, and widespread doesn’t mean acceptable.
Consider these statistics:
- Over 45% of Australian adults report inadequate sleep
- Stress-related conditions account for millions of sick days annually
- Sleep disorders affect approximately 1.5 million Australians
When nearly half the population is experiencing sleep problems, it becomes easy to think poor sleep is just “how things are” rather than recognising it as a health issue that impacts quality of life.
The Comparison Trap
We look around and see everyone else seemingly managing their stress, functioning on poor sleep, and dealing with general health concerns without professional help. This creates the illusion that we should be able to manage these issues on our own.
What we don’t see is the hidden cost of this “management”—the reduced performance, the relationship strain, the decreased enjoyment of life, and the long-term health implications of leaving these issues unaddressed.
Professional and Social Pressure
There’s an unspoken expectation that adults should be able to handle sleep problems, stress, and general health concerns independently. Seeking professional help for these issues can feel like admitting failure or weakness.
This mindset is not only unhelpful—it’s actively harmful. It prevents people from accessing care that could significantly improve their quality of life and prevent more serious problems from developing.
The Emergency Medicine Mindset
Our healthcare system has historically been designed around crisis intervention rather than preventive care. This has created a mental model where medical attention is only warranted for serious, acute problems.
But this emergency medicine mindset doesn’t match how most health issues actually develop. The majority of chronic health problems start as manageable concerns that gradually worsen without intervention.
The Hidden Scale of “Minor” Problems
Let’s put these “minor” issues in perspective. Sleep problems, stress, and general health concerns aren’t rare or unusual—they’re epidemic.
The Sleep Crisis
Australia is experiencing a sleep crisis that we’ve collectively decided to ignore:
- 45% of adults report inadequate sleep affecting their daily functioning
- Sleep disorders contribute to workplace accidents, errors, and reduced productivity
- Poor sleep is linked to increased risk of cardiovascular disease, diabetes, depression, and immune dysfunction
- The economic cost of sleep disorders in Australia is estimated in the billions annually
These aren’t “minor” problems—they’re public health issues with serious individual and societal consequences.
The Stress Epidemic
Stress has become so normalised that we’ve forgotten what normal stress levels actually feel like:
- Chronic stress is linked to virtually every major health condition
- Stress-related mental health issues are the leading cause of workplace disability
- The majority of GP visits involve stress-related symptoms or conditions
- Stress impacts immune function, digestive health, cardiovascular health, and cognitive performance
When something affects this many aspects of health and wellbeing, calling it “minor” becomes absurd.
The General Health Blind Spot
Those vague feelings of not being quite right—low energy, frequent minor illnesses, difficulty concentrating, mood fluctuations—represent a massive blind spot in how we think about health.
These symptoms often signal that your body’s systems are under strain and struggling to maintain optimal function. Dismissing them as “just getting older” or “just how life is” means missing opportunities for intervention that could significantly improve quality of life.
The Compound Effect: When Small Issues Become Big Problems
Here’s where the real cost of dismissing “minor” issues becomes clear: these problems rarely stay minor, and they rarely resolve themselves.
The Escalation Pattern
Sleep problems don’t just affect your energy levels—they set off a cascade of health impacts:
- Poor sleep increases stress hormones, making it harder to cope with daily challenges
- Elevated stress affects immune function, leading to frequent minor illnesses
- Compromised immune system and chronic stress affect mood and cognitive function
- Mood and cognitive impacts affect work performance and relationships
- Relationship and work stress further disrupts sleep, completing the cycle
What started as “just trouble sleeping” has now become a complex web of interconnected health issues.
The Prevention vs Treatment Economics
Here’s the financial reality: addressing sleep, stress, and general health concerns early is almost always more cost-effective than waiting until they escalate.
Early intervention might involve:
- Professional consultation to identify contributing factors
- Lifestyle modifications guided by expert advice
- Stress management strategies tailored to your situation
- Sleep hygiene improvements based on professional assessment
Late intervention often requires:
- Multiple specialists to address different symptoms
- Medication management for chronic conditions
- Time off work for more serious health issues
- Relationship counselling for stress-related conflicts
- Intensive treatments for conditions that could have been prevented
The economic argument for early intervention is compelling, but the quality of life argument is even stronger.
Real-World Escalation Examples
Consider these common progression patterns:
Sleep Problems → Chronic Health Issues:
- Difficulty falling asleep → chronic fatigue → immune suppression → frequent illnesses → work absences → career impacts
Stress → Physical Health Problems:
- Work stress → poor sleep → digestive issues → anxiety → relationship strain → depression
General Health Concerns → Complex Conditions:
- Low energy → poor exercise tolerance → muscle weakness → increased injury risk → chronic pain → mobility limitations
Each progression could have been interrupted with early professional consultation and intervention.
The Daily Life Tax: What “Managing” Really Costs
When we say we’re “managing” sleep problems, stress, or general health concerns, what are we actually managing? And what’s the real cost of this ongoing management?
Cognitive Performance Impacts
Poor sleep doesn’t just make you tired—it fundamentally impairs cognitive function:
- Attention and concentration decrease significantly with sleep deprivation
- Memory consolidation is impaired, affecting both short-term and long-term memory
- Decision-making abilities become compromised, leading to poor choices
- Creative problem-solving declines, affecting work performance and personal satisfaction
- Processing speed slows, making everyday tasks more effortful
These aren’t minor inconveniences—they represent a significant reduction in your mental capacity and effectiveness.
Emotional Regulation Challenges
Chronic stress and poor sleep dramatically affect your emotional stability:
- Increased irritability strains relationships with family, friends, and colleagues
- Reduced patience affects your ability to handle normal daily frustrations
- Mood swings create unpredictability in your emotional responses
- Anxiety and worry become disproportionate to actual problems
- Depression and hopelessness can develop as coping resources become depleted
The social and relationship costs of these emotional impacts can be substantial.
Physical Symptoms That Compound
The physical manifestations of poor sleep and chronic stress aren’t just uncomfortable—they’re signals that your body is struggling:
- Headaches and muscle tension that require constant management
- Digestive issues that affect nutrition and comfort
- Frequent minor illnesses that disrupt plans and productivity
- Low energy and fatigue that limit your capacity for activities you enjoy
- Physical discomfort that affects sleep, creating a vicious cycle
Each symptom requires mental and emotional energy to manage, creating a constant drain on your resources.
The Relationship and Work Performance Tax
The impacts of unaddressed sleep, stress, and health concerns extend far beyond personal discomfort:
Work Performance:
- Reduced productivity and accuracy
- Increased absenteeism and sick days
- Difficulty meeting deadlines and commitments
- Strained relationships with colleagues and supervisors
- Limited capacity for career advancement
Personal Relationships:
- Increased conflict and misunderstandings
- Reduced patience with family members
- Withdrawal from social activities and friendships
- Decreased intimacy and connection with partners
- Inability to be fully present in important moments
These impacts have lasting consequences that extend far beyond the initial health concerns.
When “Normal” Becomes Problematic
One of the biggest challenges in addressing sleep, stress, and general health concerns is distinguishing between temporary, manageable issues and problems that warrant professional attention.
Understanding the Difference Between Temporary and Chronic
Everyone experiences periods of poor sleep, increased stress, or feeling less than optimal. The question is: when do these temporary experiences become chronic patterns that deserve professional attention?
Consider these indicators:
Temporary (usually manageable independently):
- Sleep difficulties lasting less than 2-3 weeks
- Stress related to specific, time-limited situations
- Health concerns that improve with basic self-care
- Issues that don’t significantly impact daily functioning
- Problems that resolve when circumstances change
Chronic (likely to benefit from professional consultation):
- Sleep problems persisting for more than a month
- Stress that continues despite removal of initial triggers
- Health concerns that worsen or persist despite self-care efforts
- Issues that significantly impact work, relationships, or daily activities
- Problems that create anxiety or worry about underlying causes
Red Flags That Suggest Professional Consultation
Certain patterns and symptoms suggest that professional input could be particularly beneficial:
Sleep-Related Red Flags:
- Difficulty falling asleep most nights for several weeks
- Waking frequently during the night
- Waking much earlier than intended
- Feeling unrefreshed despite adequate sleep time
- Daytime fatigue affecting work or safety
Stress-Related Red Flags:
- Physical symptoms of stress (headaches, muscle tension, digestive issues)
- Stress that doesn’t improve with rest or time off
- Difficulty “switching off” from worries
- Stress affecting sleep, appetite, or relationships
- Feeling overwhelmed by normally manageable situations
General Health Red Flags:
- Persistent low energy despite adequate rest
- Frequent minor illnesses or slow recovery
- Unexplained changes in mood, appetite, or sleep patterns
- Physical symptoms that interfere with daily activities
- Concerns that create anxiety or worry
The key principle: if health concerns are affecting your quality of life or causing ongoing worry, they deserve professional attention.
Quality of Life as a Valid Health Metric
Here’s a radical idea: you don’t need to wait until problems become severe to seek professional help. Quality of life is a legitimate health concern, and feeling your best is a worthy goal.
Professional consultation can be valuable even when issues aren’t severe:
- Validation that your concerns are reasonable and worth addressing
- Expert assessment to rule out underlying conditions
- Personalised strategies based on your specific situation and lifestyle
- Peace of mind from professional evaluation
- Prevention of more serious problems developing
The goal isn’t just treating disease—it’s optimising health and wellbeing.
The Accessibility Factor: Why Convenience Matters for “Minor” Issues
Here’s where the traditional healthcare model fails people with sleep, stress, and general health concerns: it’s designed for crisis intervention, not preventive care or quality of life concerns.
The Proportionality Problem
Traditional healthcare asks you to treat every medical consultation as a major life event worthy of significant disruption. Taking half a day off work, arranging childcare, traveling to appointments, sitting in waiting rooms—this level of effort feels disproportionate to concerns you perceive as “minor.”
The result? People postpone seeking help until problems become severe enough to justify the hassle.
How Traditional Healthcare Barriers Amplify Avoidance
The inconvenience of traditional healthcare particularly impacts “minor” issues:
- Booking delays mean concerns may resolve (or worsen) before appointments
- Time requirements feel excessive for non-urgent problems
- Waiting rooms create anxiety about “wasting the doctor’s time”
- Rushed consultations don’t allow for thorough discussion of lifestyle factors
- Limited follow-up means ongoing support is difficult to access
Each barrier reinforces the message that these concerns aren’t important enough to address.
The Role of Telehealth in Addressing “Minor” Issues
Accessible telehealth consultation changes the equation entirely:
- Proportionate effort that matches the level of concern
- Flexible scheduling that accommodates rather than disrupts your life
- Comfortable environment that reduces anxiety about seeking help
- Adequate time for thorough discussion without rushed consultations
- Easy follow-up for ongoing support and monitoring
When healthcare becomes as accessible as a phone call, the barrier to addressing concerns early disappears.
Removing the Guilt Around Seeking Help
One of the most significant benefits of accessible healthcare is removing the guilt and anxiety around seeking help for “minor” issues.
Many people worry about:
- “Wasting the doctor’s time” with non-urgent concerns
- Being judged for not managing problems independently
- Taking appointment slots from people with “real” problems
- Seeming weak or unable to cope
Accessible telehealth consultation removes these concerns by:
- Providing dedicated time for your concerns without competing with emergency cases
- Creating a comfortable environment for discussing lifestyle and wellbeing issues
- Offering professional validation that your concerns are legitimate
- Making consultation feel proportionate to the level of concern
Taking Action on What You’ve Been Dismissing
Ready to stop dismissing your health concerns as “minor”? Here’s how to start addressing the sleep problems, stress, and general health issues you’ve been managing on your own.
Practical Steps for Addressing Sleep Concerns
Sleep problems rarely resolve themselves, but they often respond well to targeted interventions:
Start with an honest assessment:
- Track your sleep patterns for a week, noting bedtime, wake time, and sleep quality
- Identify factors that seem to affect your sleep (stress, caffeine, screen time, environment)
- Note how sleep affects your next-day functioning and mood
Consider professional consultation if:
- Sleep problems persist despite basic sleep hygiene improvements
- You regularly feel unrefreshed despite adequate sleep time
- Sleep issues are affecting work, relationships, or daily activities
- You’re concerned about underlying causes of sleep difficulties
A healthcare professional can help identify contributing factors you might not have considered and provide personalised strategies based on your specific situation.
Stress Management That Actually Works
Generic stress management advice often fails because it doesn’t account for your individual circumstances, personality, and lifestyle.
Effective stress management starts with understanding:
- What specific factors are creating stress in your life
- How your body typically responds to stress
- What stress management approaches align with your preferences and schedule
- Whether underlying health factors are affecting your stress response
Professional consultation can provide:
- Personalised stress management strategies
- Assessment of whether physical factors are contributing to stress
- Guidance on when stress levels warrant additional support
- Strategies for improving stress resilience over time
When to Seek Professional Input vs Self-Help
The decision to seek professional consultation doesn’t have to be binary—you can use professional input to enhance your self-management efforts:
Self-help approaches work well when:
- Problems are clearly linked to specific, temporary circumstances
- Basic interventions (sleep hygiene, stress reduction) show improvement
- Issues don’t significantly impact daily functioning
- You feel confident in your ability to monitor and adjust your approach
Professional consultation adds value when:
- Self-help efforts haven’t produced expected improvements
- Problems seem complex or interconnected
- You’re unsure about underlying causes or contributing factors
- Issues are affecting multiple areas of your life
- You want expert guidance on prevention strategies
The goal is using professional expertise to enhance your self-care efforts, not replace them.
Building Sustainable Health Habits
Professional consultation is most effective when it supports long-term habit development rather than providing temporary fixes:
Sustainable approaches focus on:
- Gradual changes that fit your lifestyle and preferences
- Understanding the principles behind recommendations so you can adapt them
- Building systems and routines that support ongoing health
- Regular check-ins to monitor progress and adjust strategies
- Developing confidence in managing your health proactively
This approach creates lasting improvements rather than temporary symptom relief.
The Relief of Professional Validation and Guidance
One of the most immediate benefits of professional consultation is often psychological rather than medical:
- Validation that your concerns are legitimate and worth addressing
- Clarity about what you’re dealing with and why
- Direction on effective approaches tailored to your situation
- Reassurance about normal vs concerning symptoms
- Confidence in your ability to improve your health and wellbeing
This psychological relief often provides immediate benefits even before implementing specific recommendations.
Redefining What Deserves Attention
It’s time to challenge the artificial hierarchy that labels sleep problems, stress, and general health concerns as “minor” issues unworthy of professional attention.
The Investment Perspective
Think of addressing these concerns as preventive investment rather than treatment of existing problems:
- Early intervention prevents minor issues from becoming major problems
- Professional guidance helps you work smarter, not harder, on health improvements
- Quality of life improvements have value that extends far beyond immediate health benefits
- Prevention is almost always more effective and less costly than crisis intervention
The return on investment for addressing “minor” health concerns is typically substantial and immediate.
Accessibility Changes Everything
When healthcare becomes convenient, timely, and accessible, addressing health concerns early becomes the logical choice rather than the difficult one.
Accessible telehealth consultation means:
- Professional input is proportionate to your level of concern
- You can address issues before they escalate or create anxiety
- Quality of life concerns receive the attention they deserve
- Prevention becomes practical and achievable
- Healthcare supports your life rather than disrupting it
Your Health Concerns Are Valid
If sleep problems, stress, or general health concerns are affecting your quality of life, causing worry, or interfering with your daily activities, they deserve attention—regardless of whether others might consider them “minor.”
Your wellbeing matters. Your peace of mind has value. And the issues you’ve been dismissing may be having a bigger impact on your life than you realise.
The consultation you’ve been postponing because your concerns don’t seem “serious enough” might be exactly what you need to reclaim your energy, reduce your stress, and improve your overall quality of life.
Professional healthcare isn’t just for emergencies—it’s for optimising your health and wellbeing so you can live your best life.
This article provides general health information and should not replace professional medical advice. If you have specific health concerns, please consult with a qualified healthcare practitioner. All consultations should be conducted with AHPRA-registered medical professionals.